Lupine Publishers - Dentistry and Oral Health Care
Monday, March 2, 2020
Lupine Publishers: Lupine Publishers | Post Endodontic Pain Reduction...
Lupine Publishers: Lupine Publishers | Post Endodontic Pain Reduction...: Lupine Publishers | Journal of Otolaryngology Research Impact Factor Abstract Objective: The pur...
Sunday, March 1, 2020
Lupine Publishers | Oral Hygiene Habits and Dental Treatment Needs of Children with Dental Fluorosis and Those Without Dental Fluorosis Aged 12-15 Years In in a High Fluoride Area in North Kajiado Kenya
Lupine Publishers | Journal of Oral Healthcare
Abstract
Background: The dental disease identified as dental caries,
periodontal, gingival lesions and dental fluorosis when diagnosed
early and the treatment needs assessment with patients’ perception
ensures the proper use of the physical facilitates, It also
enhances planning for rational health resource allocation, utilization
and personnel distribution so as to tackle the health problems
in a holistic way.
Objective: The objective of the study was to determine the dental treatment needs among children aged 13-17 years affected by
dental fluorosis and those not affected by dental fluorosis in Kajiado North District of Kenya
Materials and Methods: Study design this was a cross sectional
comparative study of the dental treatment needs among two
age matched population groups in primary school children. Sampling and
Sample size. Stratified random sampling was used to
select four primary schools out of the primary schools in North Kajiado.
All children in the school with a full permanent dentin and
whose parents had signed the consent form were recruited into the study.
The study involved 248 children, 98(40%) males and
150(60%) females aged between 13 -17 years (mean age = 14.75±1.45)
selected by simple random sampling from 9 schools in
Kajiado North District which was purposively selected. They were all
clinically examined under natural light for plaque and gingival
scores using the Silness and Loe 1, Loe and Silness, dental caries was
recrded using the decayed Missing Filedl teeth (DMFT), while
gingivitis, periodontal disease and fluorosis using indices:- Silness
and Loe 1, Loe and Silness, DMFT,CPITN and TFI.
Results: The treatment needs for gingivitis were similar,
majority 218 (88%) children with fluorosis and 213 (86%) without
required oral hygiene instructions and prophylaxis. There were 3(1.2%)
children who had periodontitis in the group with dental
fluorosis and required scaling and root planning. There were 50%
children with caries in the fluorosis group who required one
surface and 24.2% for two surface amalgam/composite restorations and for
those without fluorosis, 76% required one surface and
15.2% two surface amalgam/composite restorations. There were 321(60.8%)
teeth surfaces which required bleaching and microabrasion
or composite masking and another 207(39.2%) for direct composite /
porcelain veneers or crowns.
Conclusion: Children with dental fluorosis were burdened more by dental disease and had more treatment needs (dental caries,
fluorosis, periodontal disease and gingivitis) when compared to those without dental fluorosis.
Introduction
Dental conditions like fluorosis, caries, gingival and periodontal
diseases require varied treatment approaches to manage them
depending on the severity hence the need to establish the levels of
disease burden and treatment needs for proper planning of dental
services. Well assessed dental treatment needs go a long way in
the estimation of resources, rational fund allocation and efficient
utilization of dental materials. Dental treatment needs should be
assessed objectively and subjectively based not only on normative
assessment but also on perceived needs and impact so as to obtain
the best outcomes. The incorporation of both the clinician’s objective
assessment and the client’s felt needs is essential in ensuring that
they participate in the general management of their condition. In
common practice today Bradshaw (1978) in a study on the problems
and progress in medical care said that the treatment needs of most
dental conditions are based on the clinician’s judgement using
the recommended dental indices1. The age between 13-17 years
forms the transition period between childhood and adulthood.
The growth changes seen during this stage of life warrants a clear
understanding of the health needs in general and support for
optimal psychosocial and emotional development. Welbury pointed
out that children affected by fluorosis suffer from low self - esteem,
social stigma and poor performance in school.
Facial image is an important aspect with regard to an individual’s
presentation and self-esteem in communication. This is greatly
affected by the presence of dental fluorosis among other things
like mal-aligned teeth, missing anterior teeth or even congenital
malformations of the oral cavity. Globally there is often a permanent
stigma associated with dental fluorosis among children or adults. A
study conducted in Brazil by Rodriques showed esthetic changes
in the permanent dentition are the greatest concern in dental
fluorosis. Studies by Welbury and Glasser have observed that if left
untreated, dental fluorosis causes embarrassment, psychosocial
distress, difficulties in societal adjustment, damage to self-esteem
and poor performance for the school-going children. Another study
in Kenya by Mwaniki showed that between 60.4% and 84.3% of the
respondents viewed dental fluorosis as a problem because of its
unfavourable effects on an individual’s personality. It is important
to note that dental fluorosis leads to shyness in expression thereby
masking the true personality of an individual. It is further evidenced
by a South African study by Mothusi that showed the trauma
suffered by young people with dental fluorosis to be depressing
such that they requested to have the teeth extracted and replaced
with dentures.
Generally, the quality of life is greatly affected by oral diseases,
dental fluorosis not being an exception, with a significant impact
on the 13-17- year- olds due to their delicate stage of growth
and development. Children experience appreciable impacts on
oral health related quality of life with the greatest burden being
associated with dental caries and to a lesser extent, fluorosis
according to a study in Uganda by Robinson. The aspects considered
when determining the quality of life with regard to oral diseases
using the oral impact of daily performance (OIDP index) include
eating, speaking and pronouncing clearly, cleaning teeth, sleeping
and relaxing, smiling without embarrassment, maintaining
emotional state and enjoying contact with others. A study in
Tanzania by Roman on the impact and treatment needs of dental
fluorosis where a total of 269 students with dental fluorosis aged
15-18 years (mean age 17.3) were involved, showed that a majority
(65.4)% had severe dental fluorosis (TFI 6-9) while 29.4% had TFI
4-5 and 5.2% had TFI 1-3. Most of the students in this study (92.6%)
perceived at least one (OIDP) with the most affected being smiling
at 88.1%, emotional stability 81.4%, and having contact with others
75.5%. Studies by Locker and Leake indicated that the oral health
status of at risk children and adolescents appeared to have been
poor resulting in the need for several treatments including urgent,
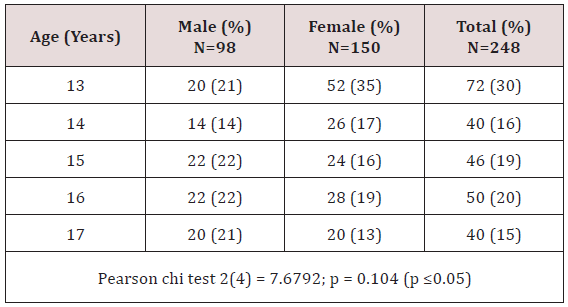
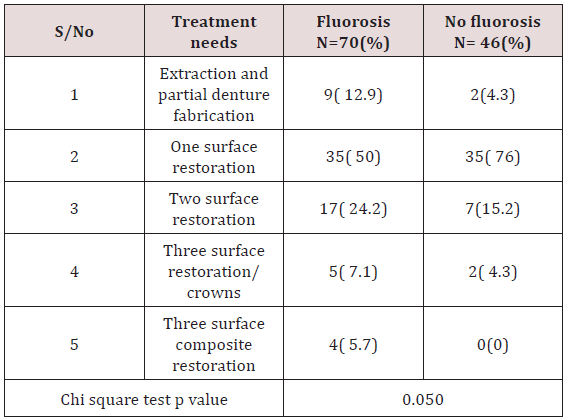
restorative, periodontal and preventive care Table 1.
Materials and Methods
Study Population
The study population comprised of 13 -17- years who were
born and brought up in Kajiado North District in the first 7 years
of life. The target population involved 34,122 children aged 13-
17 years according to the Kenyan population and housing census
2009 for Kajiado North District. The public primary and secondary
school enrolment was approximately 19,065 for the ages 13-17
years in the year 2011 in the study involved 248 children, 98(40%)
males and 150(60%) females aged between 13 -17 years (mean
age = 14.75 ±1.45) selected by simple random sampling from 9
schools in Kajiado North District which was purposively selected.
They were all clinically examined under natural light for plaque
and gingival scores, dental caries, gingivitis, periodontal disease
and fluorosis using indices:- Silness and Loe 1963, Loe and Silness
1964, DMFT,CPITN and TFI. Information on biodata, consumption
of sugary snacks, brushing was collected using an interviewer
administered questionnaire. Water samples were collected for
testing for fluoride levels at the government chemist laboratories.
Data analysis
The clinical examination forms were pre-coded. The quality of
data was ensured during the entire study process especially at the
data collection point to include completeness of questionnaires,
and validity of responses. Data was de - indentified and stored in
a password protected data base with access being granted to the
statistician. Quality control through data cleaning and validation
was censured by counter checking frequencies in the computer and any
missing data was re - entered. The findings from the study were
organized in the form of frequency tables and figures. Computations
to calculate disease burden (caries experience, prevalence of
gingivitis and periodontitis, treatment needs and the cost of
treatment) were done. The independent variable for this analysis
was presence/absence of fluorosis while the dependent variables
were age, gender, gingivitis, periodontitis, caries experience and
cost of treatment. The confounding factors were snacking and oral
hygiene practices. For categorical variables association between
dependent variables and fluorosis was tested using a Pearson
Chi-square test while a student t-test was used for continuous
variables and the conventional P value of cut-off of < 0.05 was used
to establish a significant association. To calculate the total DMFT,
the total number of teeth per child with caries, filled due to caries,
missing due to caries was summed up. For the mean gingival and
plaque scores, the total score per child was calculated by summing
the individual tooth scores, divided by 6 and the total for the index
teeth added and divided by 6. To determine the agreement rates
between assessors, a Cohen kappa score (agreement rate) was
calculated for each assessment (tooth and surface) for all children
assessed. A median agreement rate was then computed from all
individual scores calculated. Data collected was analyzed using
statistical package for social sciences (SPSS version 17.0) Table 2.
Results
Socio demographic characteristics
This study involved 248 children aged between 13-17 years
with a mean age of 14.75 years (±1.45 SD) who were all matched
for age and gender. The ratio of children with dental fluorosis and
those without was 1:1 and the male to female ratio was 2:3 and was
not statistically significant [p= 0.104 (p ≤0.05)] as shown in Table
1. There were 241 (97%) participants born and raised in Kajiado
North while 7(3%) moved to the district before 7 years of age.
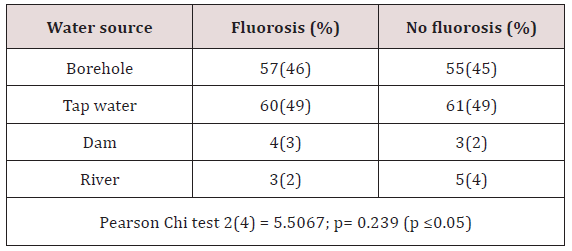
Source of water and analysis
There was a similar pattern on the water sources which was
not statistically significant [p=0.239 (p≤0.05)] for children with
fluorosis and those without fluorosis. Most of the study participants
consumed borehole water and most of tap water was also from
boreholes. Dams and river sources were for a minority group as
shown in Table 3.
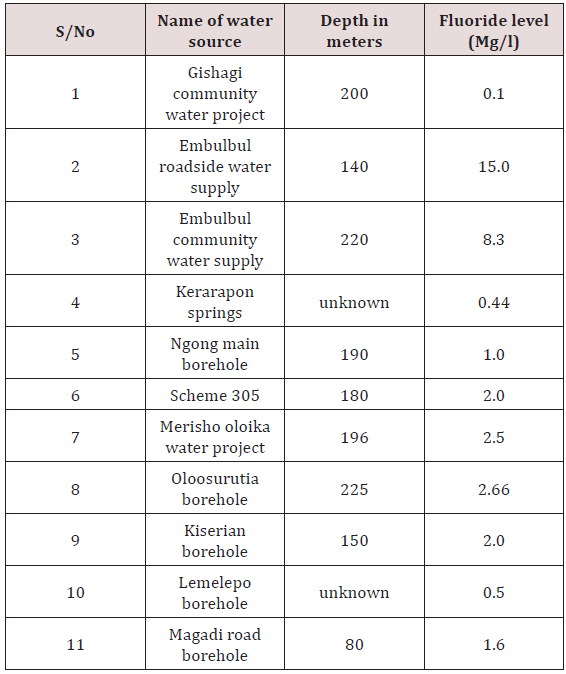
Gishagi borehole which is in a raised ground recorded low
fluoride levels of 0.1 ppm as well as Kerarapon springs 0.44 and
Lemelepo borehole 0.5, Ngong main borehole had the recommended
levels by WHO of 1ppm. Embulbul roadside and Embulbul
community water supplies had very high levels of fluoride at 8.3
and 15ppm (Table 4).
Tooth brushing habits
Majority of the children 122(98%) from each group brushed
their teeth, the frequency of brushing was similar where by
113(93%) with fluorosis and 105(88%) without used a toothbrush
while a chewing stick was used by a few (Table 5). The type of tooth
brushing aid used was not statistically significant p=0.120(p≤ 0.05).
Majority brushed once a day either in the morning after breakfast
61(50%) and 59(48%) or in the evening after meals 49(40%) and
51(42% for the children with fluorosis and those without fluorosis
respectively. Only a small percentage brushed their teeth twice a
day. There was no statistical significant difference on the timing of
brushing between the groups [p=0.180(p≤ 0.05].
Relationship between brushing habits and plaque scores
Generally, children who brushed once after breakfast in both
groups had PSs which were statistically significant p=0.003(p≤0.05)
and the children with fluorosis had the lowest PSs of 0.85(0.5).
The other brushing timings were not statistically significant
p=1.02(p≤0.05) for at night and p= 0.664(p≤0.05) for twice a day
as depicted in.
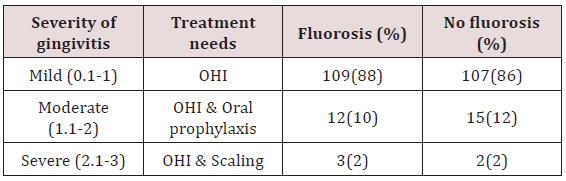
Gingivitis
Both groups had a similar pattern of treatment needs. There
were 109(88%) for OHI, 12(10%) OHI and oral prophylaxis, 3(2%)
OHI and scaling for children with fluorosis. Those without fluorosis,
107(86%) OHI, 15(12%) OHI and oral prophylaxis, 2(2%) OHI and
scaling.
Periodontitis
Of the 3(2.4%) children with fluorosis who had periodontitis
they all required scaling and root planing.
Dental caries
In both groups, dental restorations in form of one surface fillings
were mostly indicated as 35(50%)/ 35(76%) for the children
with fluorosis/those without. Two surface restorations 5(7.1%)
for fluorosis and 7(15%) those without fluorosis. Extraction and
partial dentures 9(12%) for fluorosis and 2(4.3%) those without
fluorosis. Three surface composite restorations among children
with fluorosis were 4(5.7%).
Caries experience in relation to consumption of sugary snacks
In the group with fluorosis the children who consumed sugary
snacks twice had a higher DMFT of 0.71(1.4) while children
without dental fluorosis and consumed four times scored highest
DMFT of 0.83(0.9). On the weekly snack consumption, those who
sacked once had no caries in both groups p=0;000(p≤0.05) which
was statistically significant while the highest DMFT was recorded
in those who snacked twice/four times for the fluorosis group at
0.64/0.6 while in the group without fluorosis the scores ranged
between 0.17-0.25 despite different weekly snacking times.
None of the children who brushed twice had dental caries
experience in the fluorosis group for once a day (after breakfast or
at night) had a DMFT of 0.5(1)/ 0.73(1.6). For the group without
fluorosis, there was some caries experience despite the timings for
brushing. Generally there was no statistical significant difference on
the brushing timing for both groups. The children who brushed after
breakfast had a p=0.850(p≤0.05), at night only p=0.073(p≤0.05)
and twice a day p=0.217(p≤0.05) therefore, brushing did not have
any influence on the caries experience.
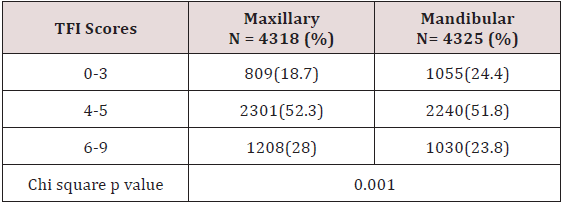
Cumulative TFI frequencies
In both jaws TFI 4-5 was the most frequent at 2301(52.3%)
on the labial and lingual surfaces of the anterior teeth in both the
maxilla and of the mandibular anterior teeth 2240(51.8%). There
were 321(60.8%) surfaces which required bleaching and/or
micro abrasion or composite masking while 207(39.2%) surfaces
required porcelain veneers or crowns Table 6.
Discussion
The current study did not find much difference in the treatment
needs for gingivitis between the two groups as majority 88%
with fluorosis and 86% without fluorosis required oral hygiene
instructions and oral prophylaxis and in periodontitis the 1.2%
affected required scaling and root planing. Most of the subjects with
dental caries required some form of restorations either one, two or
three surface amalgam/ composite restorations. A smaller number
required extractions and partial dentures. Since radiographs
were not taken for this study, it was difficult to ascertain the teeth
which were indicated for pulp therapy. Studies done in Trinidad
and Tobago by Naidu and Uganda by Nalweyiso clearly indicated
that the treatment burden of dental caries is mainly centered on
fillings, fissure sealants, pulp therapy and extractions. This study
considered treatment needs for dental fluorosis in terms of labial
surfaces from canine to canine in the maxillary teeth only. It was
established that 48% of the teeth surfaces required bleaching /
micro abrasion, composite masking and 52% for direct/indirect
composite veneers/crowns. In Kenya Mwaniki found that 60.4
- 84.3% of the respondents viewed dental fluorosis as a problem
although the study design was different from the current study.
Conclusion
Children with dental fluorosis were burdened more by dental
disease and had more treatment needs (dental caries, fluorosis,
periodontal disease and gingivitis) when compared to those
without dental fluorosis.
Read more Lupine
Publishers Blogger Articles please click on: https://lupinepublishers.blogspot.com/
Read more Lupine Dentistry Journal Blogger Articles please click on: https://lupine-dentistry-oral-health-care.blogspot.com/
Follow on Twitter : https://twitter.com/lupine_online
Friday, February 28, 2020
Lupine Publishers: Lupine Publishers | The Influence of Yoga on Traum...
Lupine Publishers: Lupine Publishers | The Influence of Yoga on Traum...: Lupine Publishers | Open access Journal of Complimentary & Alternative Medicine Abstract Sustaining a Traumatic Br...
Thursday, February 27, 2020
Lupine Publishers | Bioactivity, Biocompatibility and Biomimetic Properties for Dental Materials: Clarifying the Confusion?
Lupine Publishers | Journal of Oral Healthcare
Abstract
Often in the profession of dentistry, a new or novel instrument, material,
technique, and/or “system” is introduced which can incur a “state-of-the-art”
status without necessarily being subjected to the rigors of clinical testing or
longitudinal patient-based studies prior to receiving the stamp of approval or
the moniker of “standard of care”. Recently, provocative terminology
surrounding the field of dental materials has been publicized through the
literature, promoting exciting claims and possible long-term advancements for
patient care. In this “new era” of evidence-based restorative dentistry;
conservative interdiction, i.e. “informed” removal of diseased tissue with
concurrent substitution considering form and function, esthetics, and the
interaction of the physical and mechanical properties of the replacement
materials with living, dynamic structures found in the human tooth, has been of
paramount importance.
Abbrevations: ACP: Amorphous Calcium Phosphates, MTA: Mineral
Trioxide Aggregate, PVPA: Poly Vinyl Phosponic Acid, PAA: Polyacrylic Acids
Introduction
The progression or evolution of dentistry has occurred, to a great degree,
in concert, with the development of material technology [1]. During the last
two decades, the categorization of dental materials, specifically, adhesive
systems and composite resins have included the term “nanotechnology” into the
lexicon of scientific literature [2]. Nanotechnology involves the science and
engineering of functional molecules at the nanoscale (onebillionth of a meter)
level [2]. As applied to dentistry, this innovative approach promotes the
incorporation or interaction of nanostructured materials together with the
complex arrangement of organic/inorganic molecular-level constituents
comprising living tooth structure, allowing for a myriad of possible preventive
and therapeutic applications [2]. Owing to this progression of material
development, the assignments of additional revolutionary dimensions have
included the origination of the concepts of biocompatibility or bioactivity into
dental science.
As a possible expansion of nanotechnology applied to dental materials: the
terms biocompatible, bioactive, bioinduction, and biomimetics can be defined
independently; however, have often been characterized synonymously [3].
Biocompatible is simply a term to describe a substance or material that will do
no harm to existing living structures, that is non-mutagenic and noncytotoxic.
The term “bioactivity” was first described in 1969 by Hench, whereby a
“bioactive material is one that elicits a specific biological response at the
interface of the material which results in the formation of a bond between the
tissues and the material” [4]. Furthermore, the definition was refined and
updated to include two categories based upon intent and procedure, originally
pertaining, specifically, to bone tissue:
a) Class A: A material that elicits an intracellular and extracellular
response (osteoproductive);
b) Class B: Materials eliciting an extracellular response only
(osteocontuctive) [5].
Accordingly, a bioactive material can have “the effect on, or eliciting a
response from living tissue, organisms, or cells”, thus contributing to the
formation of a new substance or creation of a living, compatible system [3]. A
bioinductive property is defined as “the capability of a material for inducing
a response in a biologic system”[3]. Biomimetics is the “study of formation,
structure, or function of biologically produced substances and materials and
biological mechanisms and processes for the purpose of synthesizing similar
products by artificial mechanisms that mimic natural substances”[3,6]. So,
although these terms seem to imply different connotations, what can a dental
practitioner conclude, deduce, and/or apply for everyday use? Any substance,
arrived from by any process (bioactive, bioinduction, biomimetic) should
exhibit attributes of being biocompatible. It appears that both a bioactive and
biomimetic substance can include the process of bioinduction and that a
biomimetic substance could possibly be produced through bioactive activities.
Bioactive materials and processes are probably the most applicable for
endodontics and restorative dentistry based upon current uses: luting cements,
pulp capping agents, root repair materials, permanent restorations, hard tissue
remineralization (fluoride, calcium, and phosphate ions) and bone regeneration
properties, and treatment of dentinal hypersensitivity[1,3,7-13]. In order for
these materials to become biocompatibily active or retain characteristics of
bioactivity; bactericidal and bacteriostatic (inhibits bacterial growth and
biofilm formation) properties for the stimulation of reparative dentin
formation and maintenance of pulpal vitality must be achieved and maintained
[3]. Examples include fluorides for remineralization, antibacterial resins and
cements (Reactimer bond™ Shofu Dental Corp., Kyoto, Japan; ABF™ Kuraray,
Kurasiki, Japan), restoratives (Active™ BioACTIVE, PULPDENT Corp., Watertown,
MA, USA) releasing fluorides and containing amorphous calcium phosphates [ACP],
medicaments (mineral trioxide aggregate [MTA] and bioaggregate; Biodentine™,
Septodont, Lancaster, PA, USA; TheraCal™, Bisco Dental Products, Schaumburg,
ILL, USA; and Endosequence root repair [RRM]™, Brasseler USA, Savannah, GA),
and luting cements (Ceramir Crown & Bridge, Doxa Dental Inc., Chicago, ILL,
USA) that induce healing and/or for creation of new tooth
structures[1,3,7,8,10-14]. Biomimetic substances include the usage of
polyvinylphosponic acid (PVPA) polyacrylic acids (PAA) as calcium phosphate
matrix protein analogues for remineralization purposes [7,15].
Conclusion
Although these materials are in their infancy, with long-term efficacy based
on improvements of mechanical and physical properties pending, future materials
will hopefully create circumstances for increased tooth-like attributes due to
properties of adhesion, remineralization, and integration [1,3,7].
Read more Lupine
Publishers Blogger Articles please click on: https://lupinepublishers.blogspot.com/
Read more Lupine Dentistry Journal Blogger Articles please click on: https://lupine-dentistry-oral-health-care.blogspot.com/
Follow on Twitter : https://twitter.com/lupine_online
Tuesday, February 25, 2020
Lupine Publishers: Lupine Publishers | Hypertrophic Cardiomiopathy in...
Lupine Publishers: Lupine Publishers | Hypertrophic Cardiomiopathy in...: Lupine Publishers | Journal of Cardiology & Clinical Research Abstract Hypertrophic cardiomyopathy (HCM) is the most co...
Monday, February 24, 2020
Lupine Publishers: Lupine Publishers | We Hear With our Brain as the ...
Lupine Publishers: Lupine Publishers | We Hear With our Brain as the ...: Lupine Publishers | Journal of Otolaryngology Research Impact Factor Abstract There are some stu...
Lupine Publishers | Down’s Syndrome- A Disease Caused By Genetic Alteration
Lupine Publishers | Dentistry Open Access Journal
Abstract
Down’s syndrome is the most common syndrome, medical professional
encounters in day to day practice. It is a genetic disorder
with a typical face profile and few classical intraoral features. Herein
we report case and review on Down’s syndrome with facial
features.
Keywords: Down’s Syndrome; Trisomy; Chromosome; Oral Manifestation
Introduction
Down syndrome is one of the commonest disorders with huge
medical and social cost. DS is associated with number of phenotypes
including congenital heart defects, leukemia, Alzheimer’s disease,
Hirsch sprung disease etc. [1]. Down syndrome is a prevalent
genetic disorder in intellectual disability in India. Its prevalence in
tribal population is not known [2]. Down syndrome is one of the
leading genetic causes of intellectual disability in the world. DS
alone accounts 15-20% of ID population across the world [3,4].
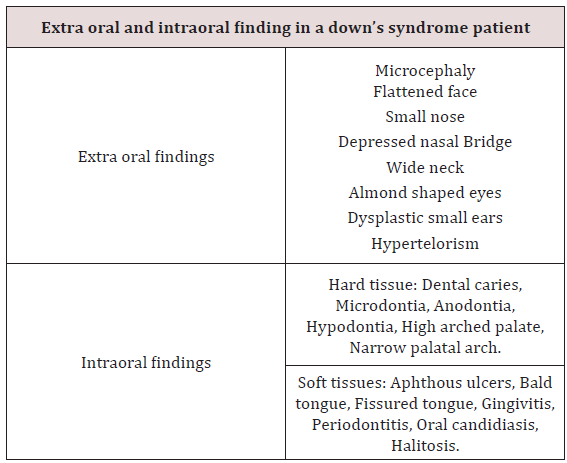
Case Report
An 8 year old male patient came to the department of oral
medicine and radiology for routine dental check-up. Extra oral
examination revealed characteristic facial profile with increased
inter canthal distance (Figure 1). Intraoral examination revealed
Gingiva was soft with deposits on the teeth, High arched palate,
with depressed nasal bridge was seen (Figure 2). Macro glossia
was also seen .Correlating the intraoral and extra oral findings a
Provisional diagnosis of Down’s syndrome/ Trisomy 21 was given.
Patient was referred to the respective departments of pedodontics
for restoration of decayed teeth.]
Discussion
Down syndrome is one of the most leading causes of
intellectual disability and millions of these patients face various
health issues including learning and memory, congenital heart
diseases, Alzheimer’s diseases, leukemia, cancers and Hirsch rung
disease. The incidence of trisomy is influenced by maternal age and
differs in population [5,6]. Facial findings in the patients can be
characterised into extra oral and intraoral features (Table 1) [7].
Parents of children with Down’s syndrome should be aware of these
possible conditions so they can be diagnosed and treated quickly
and appropriately. According to Asim A et al. A Down’s syndrome
child should have regular check-up from various consultants. These
include:
a) Clinical geneticist - Referral to a genetic counselling
program is highly desirable.
b) Developmental paediatrician.
c) Cardiologist - Early cardiologic evaluation is crucial for
diagnosing and treating congenital heart defects, which occur
in as many as 60% of these patients.
d) Paediatric pneumonologist -Recurrent respiratory tract
infections are common in patients with DS.
e) Ophthalmologist.
f) Neurologist/Neurosurgeon - As many as 10% of patients
with DS have epilepsy; therefore, neurologic evaluation may be
needed.
g) Orthopaedic specialist.
h) Child psychiatrist - A child psychiatrist should lead liaison
interventions, family therapies, and psychometric evaluations.
i) Physical and occupational therapist.
j) Speech-language pathologist.
k) Audiologist.
l) Paediatric dentist.
Hackshaw AK et al in their study, proposed a new screening
method in which measurements obtained during 1st and 2nd
trimester are integrated to provide the risk status of having
pregnancy with DS. Moderate to severe intellectual disability occur
as a constant feature, with IQ’s ranging from 20 to 85 [8]. Kennard
in his review stated that there are a number of ultrasound markers
in Down’s syndrome which includes nuchal fold thickness, cardiac
abnormalities, duodenal atresia, femur length & pyelectasis [9].
The signs and symptoms of Down’s syndrome are characterised
by neotenization of brain and bodies. Management strategies
such as early childhood intervention, screening from common
problems, medical treatment when indicated, a conductive family
environment and vocational training can improve the overall
development of children with Down’s syndrome [10].
Conclusion
Genetics have always have played a major role in physical
and mental being of an individual. Downs patients being mentally
and medically weak, best care needs to be taken with adequate
precautions.
Read more Lupine
Publishers Blogger Articles please click on: https://lupinepublishers.blogspot.com/
Read more Dentistry Open Access Journal Articles please click on: https://lupine-dentistry-oral-health-care.blogspot.com/
Subscribe to:
Comments (Atom)
Lupine Publishers: Lupine Publishers | Post Endodontic Pain Reduction...
Lupine Publishers: Lupine Publishers | Post Endodontic Pain Reduction... : Lupine Publishers | Journal of Otolaryngology Research Impact Fac...