Friday, February 28, 2020
Lupine Publishers: Lupine Publishers | The Influence of Yoga on Traum...
Lupine Publishers: Lupine Publishers | The Influence of Yoga on Traum...: Lupine Publishers | Open access Journal of Complimentary & Alternative Medicine Abstract Sustaining a Traumatic Br...
Thursday, February 27, 2020
Lupine Publishers | Bioactivity, Biocompatibility and Biomimetic Properties for Dental Materials: Clarifying the Confusion?
Lupine Publishers | Journal of Oral Healthcare
Abstract
Often in the profession of dentistry, a new or novel instrument, material,
technique, and/or “system” is introduced which can incur a “state-of-the-art”
status without necessarily being subjected to the rigors of clinical testing or
longitudinal patient-based studies prior to receiving the stamp of approval or
the moniker of “standard of care”. Recently, provocative terminology
surrounding the field of dental materials has been publicized through the
literature, promoting exciting claims and possible long-term advancements for
patient care. In this “new era” of evidence-based restorative dentistry;
conservative interdiction, i.e. “informed” removal of diseased tissue with
concurrent substitution considering form and function, esthetics, and the
interaction of the physical and mechanical properties of the replacement
materials with living, dynamic structures found in the human tooth, has been of
paramount importance.
Abbrevations: ACP: Amorphous Calcium Phosphates, MTA: Mineral
Trioxide Aggregate, PVPA: Poly Vinyl Phosponic Acid, PAA: Polyacrylic Acids
Introduction
The progression or evolution of dentistry has occurred, to a great degree,
in concert, with the development of material technology [1]. During the last
two decades, the categorization of dental materials, specifically, adhesive
systems and composite resins have included the term “nanotechnology” into the
lexicon of scientific literature [2]. Nanotechnology involves the science and
engineering of functional molecules at the nanoscale (onebillionth of a meter)
level [2]. As applied to dentistry, this innovative approach promotes the
incorporation or interaction of nanostructured materials together with the
complex arrangement of organic/inorganic molecular-level constituents
comprising living tooth structure, allowing for a myriad of possible preventive
and therapeutic applications [2]. Owing to this progression of material
development, the assignments of additional revolutionary dimensions have
included the origination of the concepts of biocompatibility or bioactivity into
dental science.
As a possible expansion of nanotechnology applied to dental materials: the
terms biocompatible, bioactive, bioinduction, and biomimetics can be defined
independently; however, have often been characterized synonymously [3].
Biocompatible is simply a term to describe a substance or material that will do
no harm to existing living structures, that is non-mutagenic and noncytotoxic.
The term “bioactivity” was first described in 1969 by Hench, whereby a
“bioactive material is one that elicits a specific biological response at the
interface of the material which results in the formation of a bond between the
tissues and the material” [4]. Furthermore, the definition was refined and
updated to include two categories based upon intent and procedure, originally
pertaining, specifically, to bone tissue:
a) Class A: A material that elicits an intracellular and extracellular
response (osteoproductive);
b) Class B: Materials eliciting an extracellular response only
(osteocontuctive) [5].
Accordingly, a bioactive material can have “the effect on, or eliciting a
response from living tissue, organisms, or cells”, thus contributing to the
formation of a new substance or creation of a living, compatible system [3]. A
bioinductive property is defined as “the capability of a material for inducing
a response in a biologic system”[3]. Biomimetics is the “study of formation,
structure, or function of biologically produced substances and materials and
biological mechanisms and processes for the purpose of synthesizing similar
products by artificial mechanisms that mimic natural substances”[3,6]. So,
although these terms seem to imply different connotations, what can a dental
practitioner conclude, deduce, and/or apply for everyday use? Any substance,
arrived from by any process (bioactive, bioinduction, biomimetic) should
exhibit attributes of being biocompatible. It appears that both a bioactive and
biomimetic substance can include the process of bioinduction and that a
biomimetic substance could possibly be produced through bioactive activities.
Bioactive materials and processes are probably the most applicable for
endodontics and restorative dentistry based upon current uses: luting cements,
pulp capping agents, root repair materials, permanent restorations, hard tissue
remineralization (fluoride, calcium, and phosphate ions) and bone regeneration
properties, and treatment of dentinal hypersensitivity[1,3,7-13]. In order for
these materials to become biocompatibily active or retain characteristics of
bioactivity; bactericidal and bacteriostatic (inhibits bacterial growth and
biofilm formation) properties for the stimulation of reparative dentin
formation and maintenance of pulpal vitality must be achieved and maintained
[3]. Examples include fluorides for remineralization, antibacterial resins and
cements (Reactimer bond™ Shofu Dental Corp., Kyoto, Japan; ABF™ Kuraray,
Kurasiki, Japan), restoratives (Active™ BioACTIVE, PULPDENT Corp., Watertown,
MA, USA) releasing fluorides and containing amorphous calcium phosphates [ACP],
medicaments (mineral trioxide aggregate [MTA] and bioaggregate; Biodentine™,
Septodont, Lancaster, PA, USA; TheraCal™, Bisco Dental Products, Schaumburg,
ILL, USA; and Endosequence root repair [RRM]™, Brasseler USA, Savannah, GA),
and luting cements (Ceramir Crown & Bridge, Doxa Dental Inc., Chicago, ILL,
USA) that induce healing and/or for creation of new tooth
structures[1,3,7,8,10-14]. Biomimetic substances include the usage of
polyvinylphosponic acid (PVPA) polyacrylic acids (PAA) as calcium phosphate
matrix protein analogues for remineralization purposes [7,15].
Conclusion
Although these materials are in their infancy, with long-term efficacy based
on improvements of mechanical and physical properties pending, future materials
will hopefully create circumstances for increased tooth-like attributes due to
properties of adhesion, remineralization, and integration [1,3,7].
Read more Lupine
Publishers Blogger Articles please click on: https://lupinepublishers.blogspot.com/
Read more Lupine Dentistry Journal Blogger Articles please click on: https://lupine-dentistry-oral-health-care.blogspot.com/
Follow on Twitter : https://twitter.com/lupine_online
Tuesday, February 25, 2020
Lupine Publishers: Lupine Publishers | Hypertrophic Cardiomiopathy in...
Lupine Publishers: Lupine Publishers | Hypertrophic Cardiomiopathy in...: Lupine Publishers | Journal of Cardiology & Clinical Research Abstract Hypertrophic cardiomyopathy (HCM) is the most co...
Monday, February 24, 2020
Lupine Publishers: Lupine Publishers | We Hear With our Brain as the ...
Lupine Publishers: Lupine Publishers | We Hear With our Brain as the ...: Lupine Publishers | Journal of Otolaryngology Research Impact Factor Abstract There are some stu...
Lupine Publishers | Down’s Syndrome- A Disease Caused By Genetic Alteration
Lupine Publishers | Dentistry Open Access Journal
Abstract
Down’s syndrome is the most common syndrome, medical professional
encounters in day to day practice. It is a genetic disorder
with a typical face profile and few classical intraoral features. Herein
we report case and review on Down’s syndrome with facial
features.
Keywords: Down’s Syndrome; Trisomy; Chromosome; Oral Manifestation
Introduction
Down syndrome is one of the commonest disorders with huge
medical and social cost. DS is associated with number of phenotypes
including congenital heart defects, leukemia, Alzheimer’s disease,
Hirsch sprung disease etc. [1]. Down syndrome is a prevalent
genetic disorder in intellectual disability in India. Its prevalence in
tribal population is not known [2]. Down syndrome is one of the
leading genetic causes of intellectual disability in the world. DS
alone accounts 15-20% of ID population across the world [3,4].
Case Report
An 8 year old male patient came to the department of oral
medicine and radiology for routine dental check-up. Extra oral
examination revealed characteristic facial profile with increased
inter canthal distance (Figure 1). Intraoral examination revealed
Gingiva was soft with deposits on the teeth, High arched palate,
with depressed nasal bridge was seen (Figure 2). Macro glossia
was also seen .Correlating the intraoral and extra oral findings a
Provisional diagnosis of Down’s syndrome/ Trisomy 21 was given.
Patient was referred to the respective departments of pedodontics
for restoration of decayed teeth.]
Discussion
Down syndrome is one of the most leading causes of
intellectual disability and millions of these patients face various
health issues including learning and memory, congenital heart
diseases, Alzheimer’s diseases, leukemia, cancers and Hirsch rung
disease. The incidence of trisomy is influenced by maternal age and
differs in population [5,6]. Facial findings in the patients can be
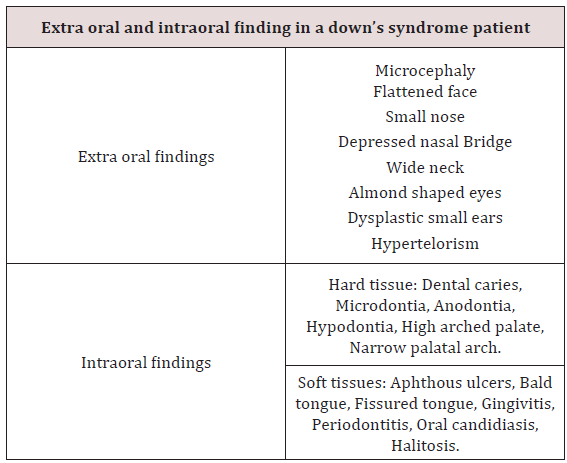
characterised into extra oral and intraoral features (Table 1) [7].
Parents of children with Down’s syndrome should be aware of these
possible conditions so they can be diagnosed and treated quickly
and appropriately. According to Asim A et al. A Down’s syndrome
child should have regular check-up from various consultants. These
include:
a) Clinical geneticist - Referral to a genetic counselling
program is highly desirable.
b) Developmental paediatrician.
c) Cardiologist - Early cardiologic evaluation is crucial for
diagnosing and treating congenital heart defects, which occur
in as many as 60% of these patients.
d) Paediatric pneumonologist -Recurrent respiratory tract
infections are common in patients with DS.
e) Ophthalmologist.
f) Neurologist/Neurosurgeon - As many as 10% of patients
with DS have epilepsy; therefore, neurologic evaluation may be
needed.
g) Orthopaedic specialist.
h) Child psychiatrist - A child psychiatrist should lead liaison
interventions, family therapies, and psychometric evaluations.
i) Physical and occupational therapist.
j) Speech-language pathologist.
k) Audiologist.
l) Paediatric dentist.
Hackshaw AK et al in their study, proposed a new screening
method in which measurements obtained during 1st and 2nd
trimester are integrated to provide the risk status of having
pregnancy with DS. Moderate to severe intellectual disability occur
as a constant feature, with IQ’s ranging from 20 to 85 [8]. Kennard
in his review stated that there are a number of ultrasound markers
in Down’s syndrome which includes nuchal fold thickness, cardiac
abnormalities, duodenal atresia, femur length & pyelectasis [9].
The signs and symptoms of Down’s syndrome are characterised
by neotenization of brain and bodies. Management strategies
such as early childhood intervention, screening from common
problems, medical treatment when indicated, a conductive family
environment and vocational training can improve the overall
development of children with Down’s syndrome [10].
Conclusion
Genetics have always have played a major role in physical
and mental being of an individual. Downs patients being mentally
and medically weak, best care needs to be taken with adequate
precautions.
Read more Lupine
Publishers Blogger Articles please click on: https://lupinepublishers.blogspot.com/
Read more Dentistry Open Access Journal Articles please click on: https://lupine-dentistry-oral-health-care.blogspot.com/
Thursday, February 13, 2020
Lupine Publishers | The Nutritional Status of the Children with Severe- ECC Comparison with the Nutritional Status of Children without Caries Aged 3-5-Years-Old and with the Caregiver’s Demographics in a Kenyan Hospital
Lupine Publishers | Dentistry Open Access Journals
Abstract
Severe early childhood caries (Severe-ECC) is an aggressive,
infectious and preventable form of dental caries that affects very
young children. The survey purposed to examine any differences in the
severity of poor nutrition in children without decay and
those children with dental decay in the age group between thirty-six and
sixty months. Sampling was purposeful and 196 children
aged between 3 to 5 years for this study. The study was hospital-based
where eighty-one children with severe dental decay who had
attended the Nyanza Provincial General Hospital (NNPGH). Similarly, one
hundred and fifteen children who were caries free were
chosen from amongst the children attending the maternal child health
clinic at NNPGH over a period of three months. Odds Ratio
(OR) and 95% Confidence Interval (CI) were used to estimate the strength
of association between Severe ECC and nutritional status.
The mean dmft for the children with severe Early Childhood Caries (ECC)
was 7.5±19. The prevalence of malnutrition was reported
among both groups of children with severe ECC and without decay as 28
(14.3%) underweight, wasting 5(2.5%), and stunting
9(4.6%). The malnutrition in children with, Severe-ECC was observed as
27(14%) underweight; 10(4.9%) of the children were
wasted, and 5(2.5%) were stunted. However among the children without
caries 26 (13.9%) were underweight while 5 (2.6% were
wasted, and 12 (6.1%) were stunted. Both children those with severe ECC
and those with decay, however, the children who were
likely to be underweight at 1.23 times were those affected with severe
ECC at 1.23 times compared to the children without decay.
Hence other factors may be playing a role in malnutrition of children
aged 3-5year old.
Keywords: Severe-ECC; Nutritional status; Caregivers demographics
Introduction
Early childhood caries (ECC) is defined as the presence of one
or more decayed (non-cavitated or cavitated lesions), those missing
(due to caries), or filled tooth surfaces in any primary tooth in a
child 71 months of age or younger. Severe Early Childhood Caries
reported in children below three years of age as smooth surface
caries1. One or more cavitated, missing teeth due to caries has
been associated with age s 3-5years.The filled smooth surfaces in
primary maxillary anterior teeth or a decayed, missing or filled a
score ≥ 4 for age 3years, a score of ≥ five is associated with 4years
while cavitation, restored tooth and missing due to caries a score of
≥6 is for children in the 5-year-old group. All these scores constitute
Severe – ECC [1].
Disadvantaged groups have been found to be vulnerable to
ECC in both developed and developing countries and even within a
single country disparity by social standing there exist, differences
due to diet, fluoride use, and social empowerment. Disparities in
social empowerment may persist due to lack of access to dental
care and inadequate utilisation of dental care even when available
[2]. Untreated caries and associated infections can cause pain,
discomfort, reduced intake of foods because eating is painful
[3]. Pain may also because the child refuses the caregiver from
maintaining good oral hygiene for the child. There is a paucity of
literature on the prevalence of Severe -ECC in Kenya. However, a
study conducted in nursery school children in Nairobi on the on
dental caries and dietary patterns reported a prevalence of 63.5%
among 3-5 years old [4]. A survey conducted in Kiambaa division in
Kiambu County, a peri-urban population, reported ECC prevalence
in 3 - 5-year-olds of 59.5% [5]. Several studies on nutritional status
and dental caries have reported variable results. A retrospective
survey on the body mass index was done in the United States of
America, and it involved two hundred and ninety-three children
aged two to five years with Severe - ECC receiving dental treatment
under general anaesthesia. In the study, the weight groups were
defined by being assigned the CDC body mass index about on age
and gender of the children. Results showed that the distribution
of subjects by percentiles and the children who were underweight
were 11%; of the study sample. However the children whose weight
was normal weight 67%; at risk of overweight 9%; overweight
11%. This study concluded that significantly, more children in the
sample were underweight than in the reference population [6].
However comparative research on the nutritional status and dental
caries among a large sample of four and five-year-old South African
children found no significant association between the prevalence of
caries and stunting or wasting. However, a relationship was found
between decayed, missing and filled surfaces and wasting [7]. This
study, therefore, aimed to compare the nutritional status of children
aged 3 – 5 years with Severe-ECC and the nutritional status of those
aged 3-5 years without caries.
Severe ECC is also associated with oral Microbiota, and in
particular anaerobic bacteria of the species Scardovia Wigggsiae
and others have been found in abundance in severe ECC lesions [8]
Materials and Methods
One hundred and ninety-six children aged between 3 to 5 years
were recruited for this study. Purposive sampling was done to select
Eighty-one children with Severe - ECC was chosen from amongst
the patients who had sought dental treatment at the dental clinic
at the Nyanza Provincial General Hospital (NNPGH). However,
115 children who were caries free were selected from amongst
the children attending the maternal child health clinic at NNPGH
over a period of three months. Inclusion criteria were: the child
was 3 – 5 years of age, was medically healthy, and the parent or
caregiver was willing to consent. A semi-structured questionnaire
was administered to the caregiver in a face to face interview, and
information was collected on the socio-demographic background
of the children. There gathered data included education level, age,
gender, and the caregiver’s, occupation, and area of residence of
the caregivers. The Intraoral examination was carried using dental
mirrors and a Michigan O dental probe under natural light as the
child sat on an ordinary chair facing the light. Severe ECC was
defined as decayed, missing or filled a score of ≥ 4 (age 3), ≥ 5 (age
4), ≥ 6 (age 5). Before dental caries diagnosis, each tooth was dried
using a piece of sterile gauze. WHO 1997 caries diagnosis criteria
were used, and dental caries was diagnosed when there was a
clinically detectable loss of tooth substance and when such damage
had been treated with fillings or extraction [9]. Anthropometric
measurements were determined to assess the nutritional status of
the children and height of the children were obtained by measuring
the child standing when standing erect and barefoot, using a
measured with a standard height board to the nearest 0.5cm. Weight
for age was measured using a Salter scale to the nearest 0.1kg. Each
parameter of height and weight had three measurements taken,
and an average of each was then recorded. The Cut-offs +2 standard
deviations (SD) were used to identify children at significant risk for
either delayed (<-2SD) or excessive (>+2SD) growth. The indicators
were weight-for-age (WAZ), height-for-weight (HAZ), weight-forheight
(WHZ) based on the World Health Organisation(WHO) 2005
recommended reference standard [10]. The collected data collected
were coded, cleaned and analysed using SPSS version 17.0 (SPSS
Inc, Chicago Illinois, USA) for Windows and Microsoft Office Excel
2007. Nutritional data was analyzed using Epi-Nutri program of
Epi-Info version 3.5.1. Descriptive statistics such as proportions
were used to summarize categorical variables while measures of
central tendency such as mean, standard deviations and ranges
were used to summarise continuous variables. The strength of
association was established between categorical values using a
Pearson’s Chi-square tests. Odds Ratio (OR) and 95% Confidence
Interval (CI) were used to estimate the strength of association
between independent variables and the dependent variable. The
multivariate analysis was done using binary logistic regression at
a statistical significance set at p≤0.05. The relevant research and
ethics approving institutions approved the study.
Results
A total of 196 children aged 3-5 years were recruited into the
study, eighty-one children with S - ECC (41.3%) and 115(58.7%)
without caries. The study group had a mean age of 4.1 + 0.6years,
and it ranged from 3- 5 years with a high proportion of the children
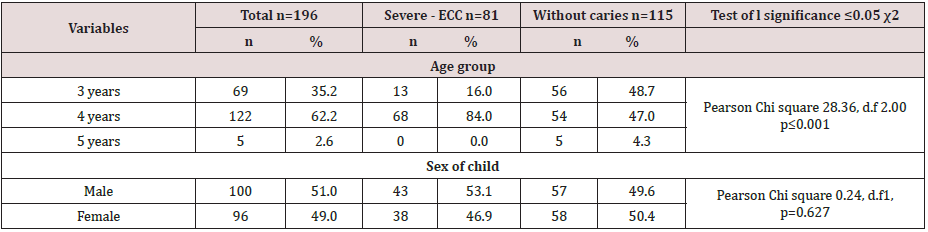
(62.2%) aged four years. There was a statistically significant
difference in age distribution among children with Severe ECC and
children without caries (χ2=28.36, d.f=2, p<0.001). The majority of
the children with caries were aged four years (84.0%) compared to
those without caries (47.0%).Gender distribution was comparable
with boys slightly more (51.0%) than girls (49.0%).
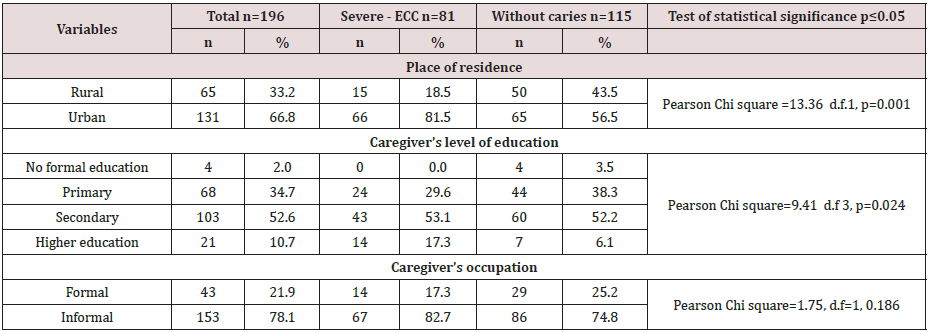
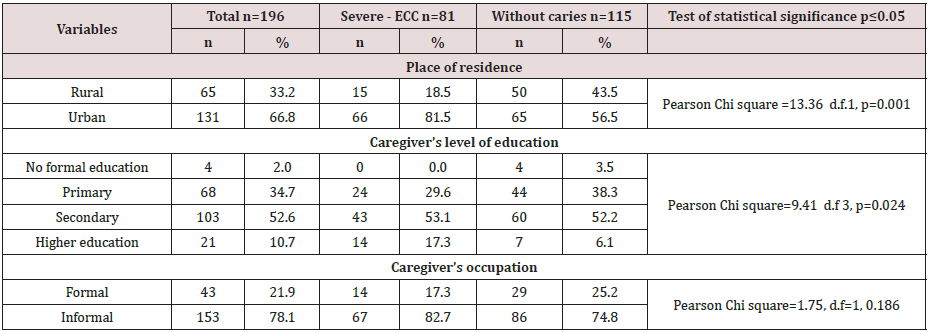
Sixty-five children (33.2%) lived in the rural community, and
131(66.8%) lived in the urban area. The differences in the area
of residence were significant with a Pearson chi square=13.36,
df=1, p≤0.001) for the children with severe ECC and those children
without decay. It was noted that sixty-six (81.5%) out of 81
children with Severe ECC lived in an urban setting when compared
to children who were caries- free who had 65 (56.5%) out of 115
children who were caries free. Some sixty-eight caregivers had
had primary school education of whom 24 (29.6% had severe ECC
while 44 (38.3%)) were caries free. However, 103 caregivers had secondary school education of whom 43 (53.1% had severe-ECC
and60 (52.2%), while 21 (10.7%) their caregivers had tertiary
education and 14 (17.3%) and seven 6.1% were caries free. Also,
children whose caregivers had a primary level of education had
the highest prevalence of severe-ECC followed by those whose
caregivers had secondary education. The differences in the severecares
prevalence were significant with a Pearson Chi-square =9.41
d.f 3, p≤0.024 Table 1 & 2.
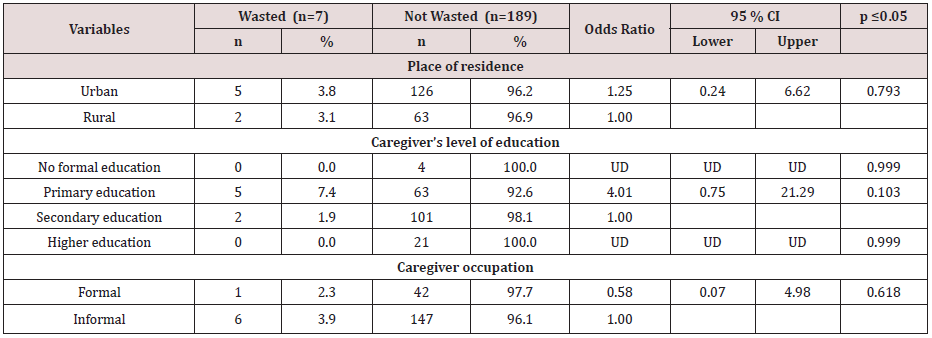
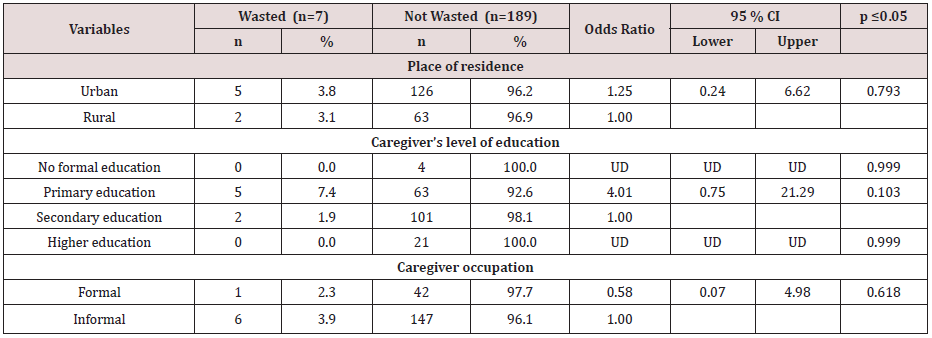
Table 2: Level of education, demographics for the caregivers, place of residence, level of education, and occupation.
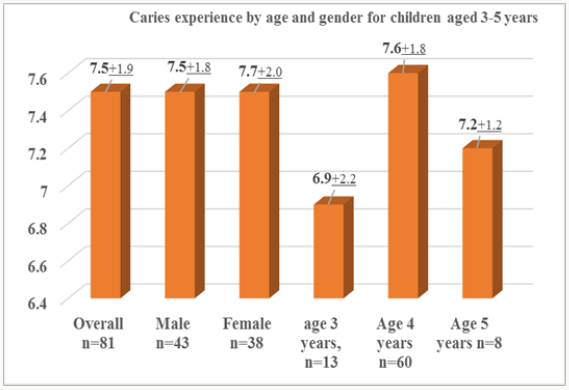
The mean dmft of 7; 5±1.9 d was observed among children with
Severe – ECC, and it ranged from 5 to 12 scores. Scores. However,
the mean dmft for the males was 7.5±1.8 and for females (7.5±2.0),
which was statistically insignificant difference found between the
two groups (t=0.15, p=0.88). The mean dmft score for children
aged three years was 6.9 ± 2.2, four years was 7.6 ± 1.9, and for
five-year-olds was 7.2 ±1.2 and all the dmft ranged from 5-12. The
dmft progressively increased with age and peaked at age four years.
There were no statistically significant differences found between
the age groups (t=1.59, p=0.248). Figure 1.
Overall the decayed component of the dmft contributed 92.3%.
The missing and filled component of the dmft contributed 7.4%
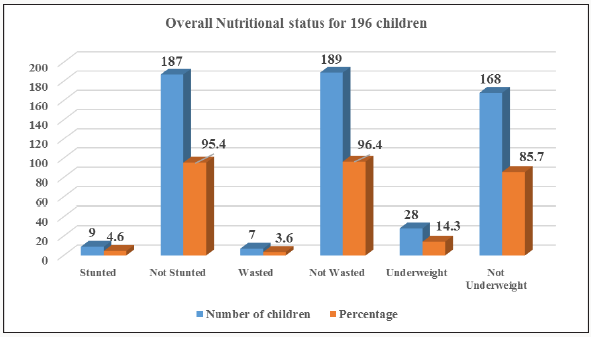
and 0.3% respectively. The overall prevalence of underweight for
acute malnutrition, stunting, and wasting for chronic malnutrition
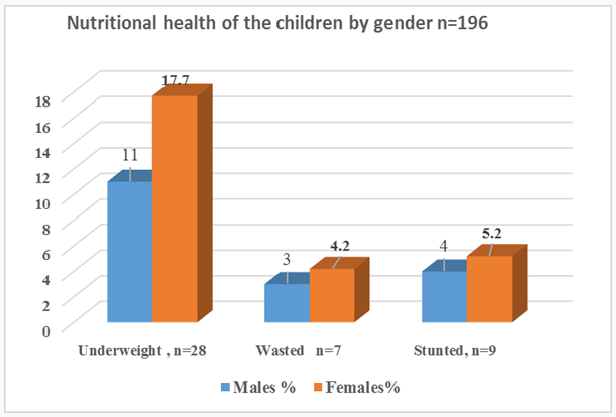
was 14.3%, 4.6%, and 3.6% respectively. There were more females
17(17.7%), 4 (4.2%), and 5 (5.2%) who were underweight,
wasted and stunted respectively when compared to males, but
this difference was not statistically significant Pearson Chi-square
respectively for underweight, stunted and wasted were 1.80,df=1,
p=0.180 ; 0.19,d. f=1, p=0.660 and 0.16, d.f=1, p=0.686 Figures 2
& 3.
Table 3: Underweight among children with caregivers place residence, level of education, and occupation.


When the caregiver’s residence, level of education, and occupation
were considered the children who lived in the rural areas had
higher prevalences of were underweight 10(15.4%), when
compared to the children in the urban areas 18(13.7%) resided in
urban areas. Sixty-eight children had caregivers whose education
was of a primary level, and 11(16.2%) of the children were
underweight while 57 (83.8%) had normal weight for age. Children
whose parents had a secondary education were 103 of whom 14
(13.6% were underweight, and 89 (86,4%) had normal weight for
an age while caregivers who had higher education were eighteen
of whom 3(14.3%) were underweight, and 15( 85.7%) had normal
weight. There were more underweight children 24(15,7) out of 153
when weight for age was examined about the caregivers who were
informally employed, However, the differences in the children who
were underweight with the caregiver’s various demographics were
not significant Table 3.
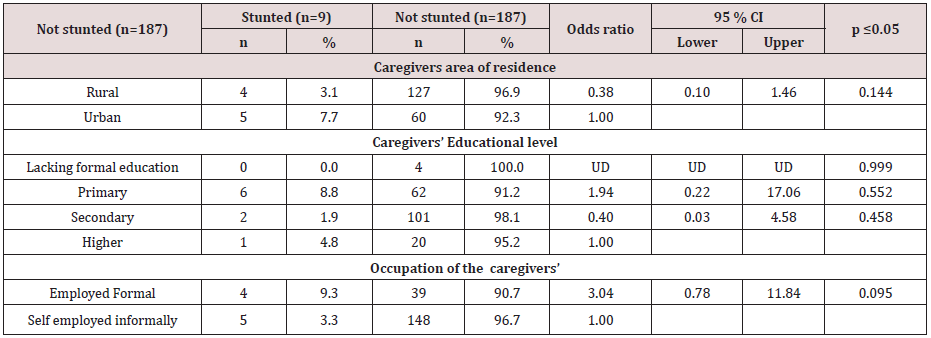
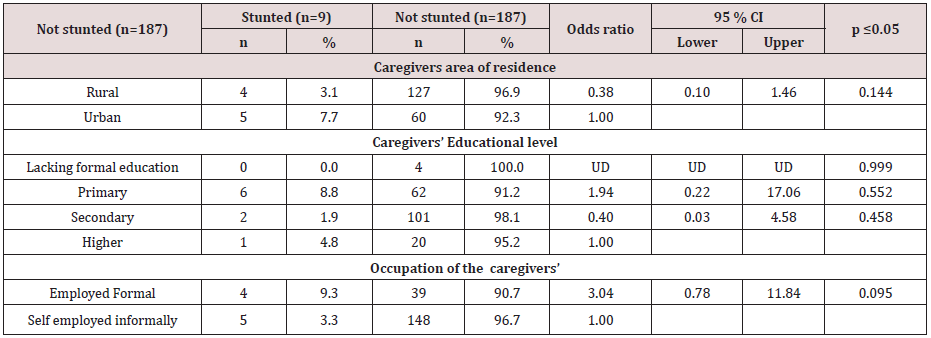
According to the educational level, the children who were
stunted and whose parents had a primary education were four
(9.3%)), secondary 6(8.8%), and higher education were 5(7.7%).
The caregivers who had formally employed were from the urban
area while those who were informally employed and had primary
school education were from the rural areas Table 4. There were
statistically insignificant differences in the caregiver’s place of
residence, the level of education, and occupation among children
who stunted and those who were not stunted.
Table 4: Stunting among children about caregivers place of residence, level of education, and occupation.
For the children who were wasted five 7.4% of the caregivers
lived in the Urban area and had a primary level of education; also
6(3.9%) of the caregivers had informal employment, and 2(3.1%)
resided in rural areas Table 5. There statistically insignificant
differences in the caregiver’s place of residence, the level of
education, and occupation among children who wasted and those
who were not wasted.
Table 5: Wasting among children about caregivers place of residence, level of education, and occupation.
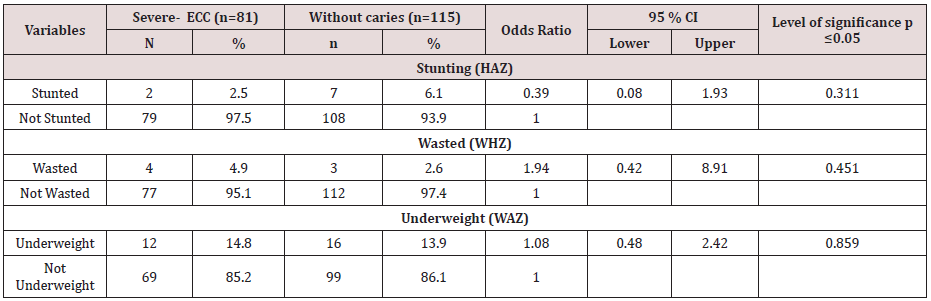
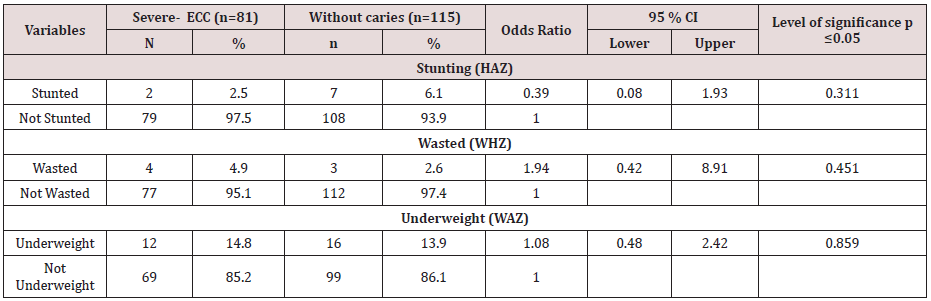
There was a slightly higher prevalence of underweight
14’8% for the children suffering from severe ECC compared with
children without decay 13.9%. Although there were differences
in the nutritional status of children with severe- ECC and children
without caries the differences were insignificant for stunting with
p=0.311; also underweight was insignificant with p=0.859 while wasting had p=0.451). A child identified with Severe- ECC at risk
1.08 more times likely to become underweight when compared to
a child who did not have decay odds ratio lower and upper limits of
0.48 and 2.4 at 95% CL Table 6.
Table 6: Comparison of the nutritional status of children with Severe ECC and children without caries.
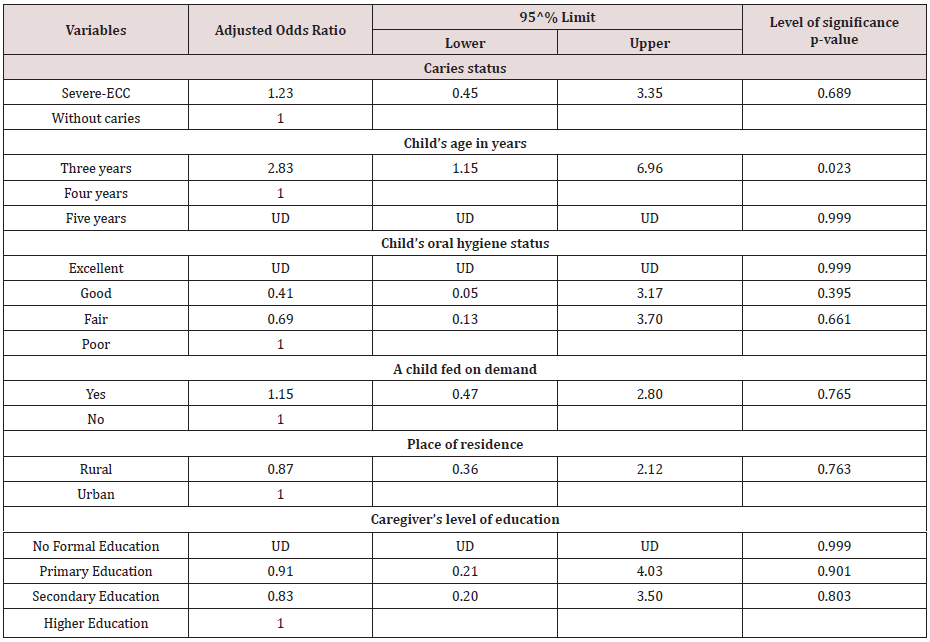
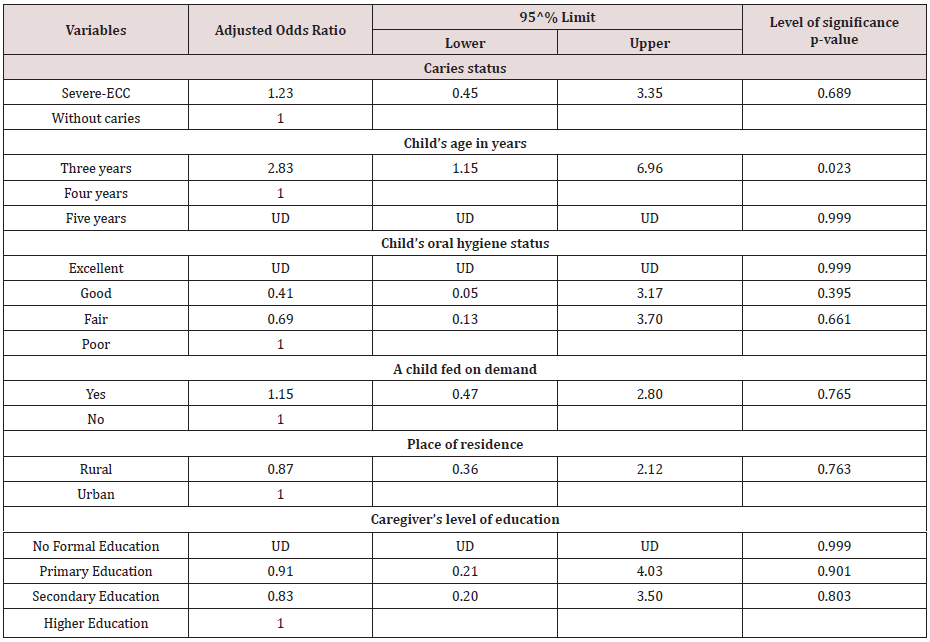
Multivariate analysis was done to determine the relationship
between underweight and Severe- ECC among the participating
children. Five factors associated with underweight and Severe-
ECC at P≤0.05 during bivariate analysis were considered for
multivariable analysis upon fitting the factors using binary logistic
regression. Adjusting for child’s age in years, child’s oral hygiene
status, child feeding on demand, place of residence and caregiver’s
level of education, the occurrence of S-ECC was not significantly
associated with underweight (AOR=1.23; 95% CI: 0.45 – 3.35;
p=0.689). However, a child with S – ECC was 1.23 times more
likely to have low weight for an age when compared to a child
who was caries – free. However adjusting for other factors, age
three years was found to be statistically significantly associated
with underweight with an Adjusted Odds Ratio value =2.83; 95%
CI: 1.15 – 6.96; p=0.023 Table 7. A child aged three years was 2.83
times more likely to be underweight when compared to one aged
four years.
Table 7: Logistic Regression Predicting underweight using caries status, Child’s age in years, Child’s oral hygiene status, Child
feeding on demand, Place of residence and Caregivers level of education.
Discussion
In the current study found that children with severe ECC were
mainly from urban areas in comparison to children who were
caries free. The finding of a high prevalence of severe –ECC in the
urban children is similar to other studies in Kenya and elsewhere
that have shown that children residing in urban areas have a
higher caries experience than their rural counterparts [4,5,11,12].
The mean dmft of children with severe ECC in the present study
was 7.5+1.9 which is comparable to a study carried out among
preschool children of low socioeconomic status in India which
reported a mean dmft of 8.9 [13]. Studies in the USA, and Canada
among preschool children found mean dmft scores of 9.6±3.6 and
10.5 respectively [13-15]. The differences in the mean dmft may be
due to variations in dietary practices among different populations.
Also, decayed component accounted for 92.3% of the dmft, and
this finding was similar to a study in South Africa [14]. Untreated
tooth decay reflects a low utilisation of oral health services or lack
and inaccessibility of preventive and curative dental services to the
caregivers, or if the facilities are available, they are too costly.
Higher caries experience was observed in the children from the
urban areas when compared to their rural counterparts [11]. The
mean dmft of children with severe ECC in the present study was
7.5+1.9. The caries experience for severe-ECC in the present study
is comparable to a study carried out in a low social, economic status
in India among preschooler and reported a mean dmft of 8.9[112].
Studies in the USA, and Canada among preschool children have
reported mean dmft scores of 9.6±3.6 and 10.5 respectively [13,14].
The differences in the dmft could be due to variations in dietary
practices among different populations. The decayed component in
the current study accounted for 92.3% of the dmft, which similar
to other studies elsewhere [14]. Untreated tooth decay reflects a
low availability and accessibility of preventive and curative dental
services.
In this study, there were more females were underweight,
stunted, and wasted when compared to males when referenced
on the WHO reference standard. However, the differences were
insignificant. The WHO child growth standards reference was used
to evaluate nutritional status. The WHO growth reference provides
a scientifically reliable yardstick of children’s growth achieved
under desirable health and nutritional conditions and establishes
the breastfed infant has been used as a reference against whom
other alternative feeding practices are measured to and compare
to regarding growth, health, and development of in children [9].
The children with severe-ECC who were underweight were 4.9%,
stunted 2.5%, and those who were wasted were 14.8%. The presence
of underweight, stunting, and wasting may be associated with the
inability of the children with severe-ECC to chew the available
food and absorb enough nutrients resulting in faltering nutritional
status. In comparison a study carried out in Italy among 2- 6 years
old found that 11% were e underweight, 11.11% overweight and
22.2% to be at risk of overweight [15]. A study in the USA reporting
on the BMI of children with severe ECC noted those who were
underweight as 11.%, overweight 11%, and those who were at risk
of overweight were nine %6. These findings were insignificant may
be due to differences in cultural, dietary practices and the primary
determinants of nutritional status among the different populations.
In Kenya, the primary determinants of nutritional status among
children under five years of age include poverty, hunger, and
drought [16]. The low weight for age observed with urban children
is similar to previous research from other countries where children
with high prevalence with severe-ECC had low weight for age [17].
Children who were malnourished were also noted to have
severe ECC compared to children who were caries free. There are
high levels of malnutrition in Nyanza as reported in the Kenya
Demographic and Health Survey 2008-2009 where 19%, 2%, and
14%of the children under five years were underweight, wasted and
stunted respectively [18]. Considering the caregiver’s demographic
factors children who had low weight for age, wasting and
stunted, resided in rural areas. Also, their caregivers had informal
employment and had a primary level of education.The finding may
be related to the low socioeconomic status and affect access to
health care, food security and hence changing overall nutritional
status [16,17].
The differences in the nutritional status of the children with ECC
and those without ECC was insignificant. South African children
aged between four and five years reported similar findings as what
has been observed in this study. Njoroge et al. reported 60% in a
study population of 338 children aged five years and below[4]. The
most affected dentition were the upper central incisors however
the severity of decay increased with age and the first and the second
deciduous molars had the highest prevalence ranging between 57%
-66%. In this study, the caregivers knew the importance of good
oral hygiene and significance of snacks about caries formation.
However, the infant feeding habits and the weaning practices were
not reported on in this study [19,20].
The South African Study found no relationship between the
prevalence stunting or wasting with dental caries. However,
they reported an association between Wasting with the decayed,
missing and filled tooth surfaces [7]. Children with severe ECC
were 1.23 times more likely to be underweight when compared to children without caries. Severe ECC may affect general health
and development because a toothache associated with caries may
affect food intake and sleep [1]. Poor oral health associated with
pain may interfere with the intake, mastication digestion of food
and nutrients which may lead to decrease in good nutritional health
and reduced quality of life for a child [1].
In summary, the difference in the nutritional status of children
with severe ECC and children without caries and stunting was
insignificant p=0.311, Underweight p=0.859 and wasting p=0.451.
However, children with Severe ECC were 1.23 .times more likely to
be underweight than children without caries.
Read more Lupine Publishers Blogger Articles please click on: https://lupinepublishers.blogspot.com/
Read more Lupine Dentistry Journal Blogger Articles please click on: https://lupine-dentistry-oral-health-care.blogspot.com/
Friday, February 7, 2020
Lupine Publishers: Lupine Publishers | Somatic Mutations in Cancer-Fr...
Lupine Publishers: Lupine Publishers | Somatic Mutations in Cancer-Fr...: Lupine Publishers | Open Access Journal of Oncology and Medicine Abstract Somatic mutations have been perceived as the causal even...
Thursday, February 6, 2020
Lupine Publishers: Lupine Publishers | Somatic Mutations in Cancer-Fr...
Lupine Publishers: Lupine Publishers | Somatic Mutations in Cancer-Fr...: Lupine Publishers | Open Access Journal of Oncology and Medicine Abstract Somatic mutations have been perceived as the causal even...
Lupine Publishers | Caregiver’s Oral Healthcare Practices And The Level of Utilisation Of Oral Health Services and The Dental Caries Experience Of 3-12-Year-Olds Suffering From Heart Disease in Nairobi, Kenya
Lupine Publishers | Dental and Oral Health Journals
Abstract
Cardiac diseases require that there is the meticulous maintenance of
oral hygiene to avoid bacteremia, which has been associated
with rheumatic heart disease and bacterial endocarditis. The aim was to
establish the utilisation of oral health care and oral health
practices of the caregiver about the oral hygiene and caries experience
of children aged 3-12 years suffering from heart disease and
were attending three pediatric cardiology clinics in Nairobi, Kenya. The
study was descriptive and cross-sectional. It involved a study
sample of children suffering from different types of cardiac conditions
and attending the Pediatric cardiac clinics in three public
institutions in Nairobi Kenya. The instruments the caregivers used to
brush the children’s teeth were the toothbrush 61(75%);
chewing stick 14(17%) and 6 (8%) never cleaned their teeth. Children who
used a chewing stick had a lower dmft of 1.40±2.98
compared to a dmft of 3.22±3.59 among children who used the toothbrush,
with Mann Whitney U, Z p=0.024 (p≤0.05).The children
who brushed their teeth had a lower mean plaque score of 1.68±0.58
compared those who did not clean with a mean plaque of
2.28±0.40 with a Mann Whitney U, Z=-2.611, p=0.009(p≤0.05). It was noted
that the children who had visited a dentist had a higher
caries experience with a dmft of 4.18±4.13 and DMFT of 1.16±1.92.
However, the children who had never sought treatment at
a dental facility had lower dmft of 1.89±2.88; and DMFT of 0.36±1, and
the differences were statistically significant with Mann
Whitney U, Z p=0.008(p≤0.05). The plaque scores and caries experience
were high in children whose caregivers had low aggregate
utilisation of the oral health care facilities. However, those who had a
low aggregate of oral hygiene practices had slightly higher
plaque scores and caries experience.
Keywords: Cardiac Disease; Children; Utilisation; Oral Health Services; Caregivers
Introduction
Populations with chronic medical illness or other disabilities
had the most unmet needs for oral health services [1], with poor
oral hygiene and increased caries experience than the general
population. For a child from a low-income family with heart
disease, this means an added economic burden in an already tricky
situation [2], as heart diseases necessitate regular dental check-ups
and maintenance of meticulous oral hygiene. This concern has even
been highlighted with new proposals on changes in the guidelines
relating to prophylaxis against infective endocarditis [3,4]. The oral
conditions may have a considerable impact on the general health
status and quality of life of otherwise healthy children, but their
effects on those children with acute and chronic illness can be more
dangerous [5]. Children with cardiac defects and diseases are at
increased risk or even life-threatening complications [6]. Hence the
need for preventive dental health care geared to reducing the risks
associated with management of the oral conditions under general
anaesthesia. Also, the prolonged bleeding from warfarin medication
often taken By the children [7-10]. Poor oral hygiene may give rise
to a frequent bacteraemia under normal physiological conditions,
and this can lead to a permanent risk of developing heart disease
[11-14]. Two common oral diseases, namely periodontal and
dental caries, though preventable, are still more prevalent in Kenya
[15,16]. The children with heart disease have the disadvantage
that their caregivers are preoccupied with the with the primary
medical condition the cardiac disease, resulting in the neglect of
other facets of the child’s total health [17]. The Kenya National Oral
Health policy document has already indicated that the dmft value
for Kenyan 5-year old children as at 2002 was 1.5±2.2, while 43%
of 6-8-year-old children had caries [15], underscoring the fact that
caries is still very rampant amongst the child population in Kenya.
The study was descriptive and cross-sectional where all the
patients aged 3 to 12 years and their caregivers attending paediatric
cardiology clinics over a three month period at Kenyatta National
Hospital (KNH), Gertrude’s Garden Children’s Hospital (GGCH) and
Mater Hospital. A Purposive sampling had been used to select the
study hospitals. Based on Kliegman. study, the study population
sample was determined as 79 cases. However, 81 patients were
recruited in the study. A semi-structured questionnaire was used
to collect information on the socio-demographic characteristics
of the children and the parent/guardian habits on oral health
practices and utilization of oral health services. As children waited
to consult the cardiologist clinical examinations done to record the
oral health status. The examination was conducted using sterilized
instruments and under natural daylight, with the participants
seated on a chair facing the window. Great care was taken during
periodontal probing for gingivitis, to avoid initiating bleeding that
could lead to septicaemia as the children were not on prophylactic
antibiotics. The results were recorded on predesigned individual
questionnaire sheets, and a record of dental caries and plaque was
done. The dental caries was then recorded as dmft for the primary
dentition and DMFT in the permanent [18,19], and the dental
plaque was marked based on the Loe and Silness plaque score
index [20]. Before commencement of the study, the examiner was
calibrated by an experienced paediatric dentist on the collection
of data relating to dental caries, and dental plaque Cohen’s kappa
index score of 0.87 and 0.85 (n=10) was obtained for dental caries
and plaque score respectively. The questionnaire was pre-tested
before use. A duplicate clinical examination was also performed
by the examiner to determine intra-examiner consistency, with
results of Cohen’s kappa index score of 0.91 and 0.86 (n=12) being
obtained for dental caries and plaque score respectively.
Data analysis
The data collected was cleaned, coded and analyzed using
SPSS version 17-computer software from SPSS Inc. IL. The results
obtained were compared and tested using Kruskal Wallis Chi-square
and Mann Whitney U statistical tests, with statistical significance
pegged at 95% confidence interval.
Results
The 81 children in the study, 44 (54.3%) were males and 37
(45.7%) females. Their ages ranged between 3-12 years with a
mean age of 8.16 years (± 2.81 SD), and the 6-9-year-olds accounted
for the most substantial proportion of 33 (40.7%) compared to
the 3-5 year-olds who formed 16(19.8%). The differences in ages
and gender were not statistically significant Chi χ2 =1.287, two
df, p=0.525(p≤0.05). A total of 37(46%) children were from rural
areas, 28(34%) were from Nairobi, and 16(20%) were from other
urban centres other than Nairobi. The distribution of the children
according to the type of heart disease, rheumatic (RHD) accounted
for 36(44.5%) while infective endocarditis (IE) affected 4(4.9%).
The duration since diagnosis of the cardiopathy ranged from less
than one year to 12 years. Nearly half of the children, 40 (49%)
had been diagnosed with the disease for a duration of between
1 to 5 years, while those who had been diagnosed more than five
years and those less than one year accounted for 30% and 21%
respectively. The caregivers’ oral health care practices that included
how the child’s teeth were brushed; the frequency of brushing; and
whether tooth brushing was supervised showed that 75(93%)
children cleaned their teeth and 6(7%) children did not clean their
teeth. Of the group that cleaned their teeth, 33(44%) did it twice a
day, 29(39%) once a day while 16% once in a while/occasionally.
About supervision, 62 (83%) reported cleaning their teeth without
supervision while 13 were assisted by the caregivers. Inquiry on the
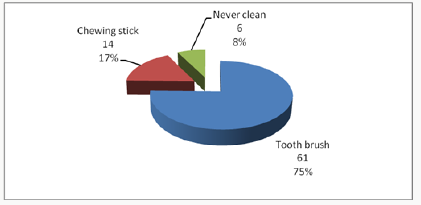
ways the child’s teeth were cleaned, 75% (61) of the children used
toothbrush and the rest of the results were as shown in Figure 1.
The children who used toothpaste were 59 (79%) while 16 (21%)
never use any toothpaste.
Considering the utilisation of oral health care services by
children with heart diseases; fifty-nine (72.8%), children had never
visited a dentist or utilised oral health services. Among the 22
(27.2%) children who had been to a dentist, the dental procedure
during the last appointment included extraction 10 (12.3%). Also
cleaning/prophylaxis (1(1.2%)), consultation ; check-up 9(11.1%)
and fillings 2(2.5%).Caregiver’s oral healthcare practices and the
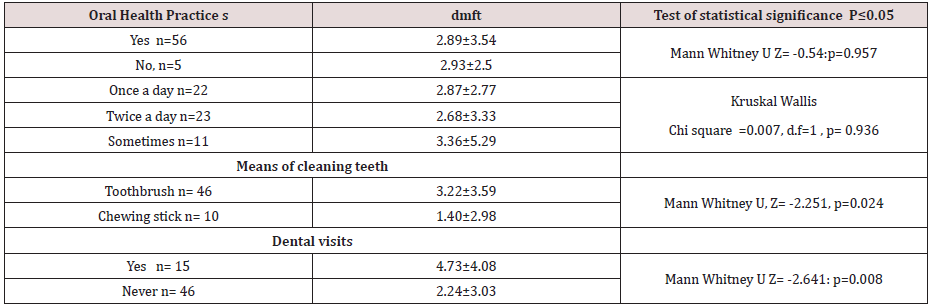
dental caries experience about the children five children who never
cleaned their teeth had a higher dmft of 2.93±2.50 compared to a
lower dmft of 2.89 ±3.54 among the 56 children who cleaned their
teeth, and the differences were insignificant with p=0.957(p≤0.05).
The differences in the frequency of tooth cleaning, the eleven
children who cleaned their teeth once in a while had a higher dmft
of 3.36±5.29 and the 23 children who cleaned twice a day had lower
dmft of 2.68±2.77, but.difference was not statistically significant
with p=0.936(p≤0.05). The children who used a chewing stick had
a lower dmft of 1.40±2.98 compared to a dmft of 3.22±3.59 among
the 46 children who used the toothbrush, with the difference was
not statistically significant, p=0.024(p≤0.05). The children who
had visited the dentist apparently had a higher caries experience
with dmft of 4.18±4.13 and DMFT of 1.16±1.92 when related to the
children who had never visited a dentist, who had lower dmft of
1.89±2.88; and DMFT of 0.36±1. These differences in the results
were statistically significant, p=0.008(p≤0.05). The rest of the
results are as shown in Table 1. When the caregivers were classified
into two groups based on the responses to the oral healthcare
practices as being favourable or unfavourable practices,53 (86%)
caregivers fell in the unfavourable oral healthcare practices. Fiftythree
children whose caregivers displayed unfavourable practices
had a higher dmft of 3.62±3.54 compared to dmft of 2.74±2.85
among the eight children whose caregivers displayed favourable
oral healthcare practices. The difference was statistically significant
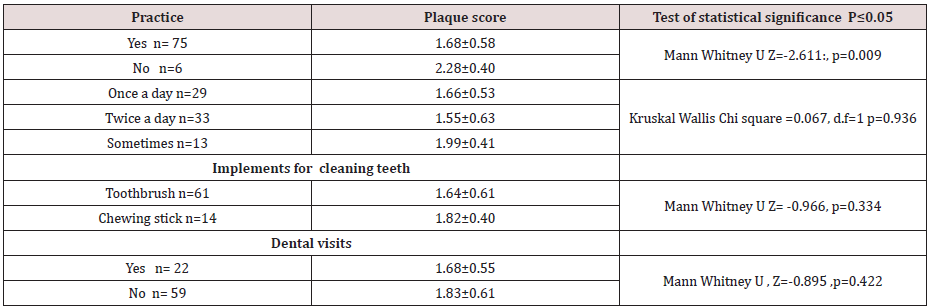
with Mann Whitney U, Z= -1.297, p=0.197(p≤0.05). The mean
plaque score was significantly lower among the 75 children
who reported to cleaning their teeth with mean plaque scores of
1.68±0.58, compared to a higher mean PS of 2.28±0.40 among the
six children who never cleaned their teeth with p=0.009(p≤0.05).
Those children who used the toothbrush had lower mean plaque
scores of 1.64±0.61. The children who cleaned more than twice
a day had the lowest mean plaque score of 1.55±0.63; and those
who cleaned their teeth occasionally had the highest mean plaque
scores of 1.99±0.41, though these differences were not statistically
significant with χ2 =0.067, 1df, p =0.936 (p≤0.05), Table 2. The
mean plaque scores among the 22 (27%) children who had been to a
dentist was mean PS of 1.68±0.55 compared to higher plaque score
of 1.83±0.61 among the 59 (73%) children who had never been to
a dentist Table 2. However, the difference was not significant, with
p=0.422 (p≤0.05)
Discussion
Despite the majority of the respondents, 75(93%), with the
majority reporting that their children cleaned their teeth, only
33(44%) of these children cleaned their teeth at least twice a
day, 62(83%), of them, cleaning their teeth without supervision
by the caregivers. Seven children had never visited a dentist to have teeth cleaned teeth cleaned. Also, some children had
occasional cleaning of their teeth, and this puts the children the
risk of developing early childhood caries, gingivitis, and poor oral
health. The poor oral health may which may give rise to frequent
transient bacteremia during mastication or tooth brushing. Other
studies among children with heart diseases have reported that 55
% of the children brushed their teeth twice a day [21,22] and that
46.1% of the children brushed three times a day. Owino et al [26]
reported that 67.5% of the 12-year-old children in a peri-urban
area brushed their teeth. Franco et, al [25] in their study considered
as disappointing the percentage of children with congenital heart
disease who had never visited a dentist, a reflection of other
results obtained in studies by Silva et al [23], Saunders et al.[18],
and Fonseca et al [5]. In this study, the very high percentage of the
children examined had never seen a dentist, with only 22(27.2%)
of the children have been to a dentist before the stu dy. Moreover,
even though, most of the treatment, which had been offered during
their visit to the dentist, was extraction, just as reported in a study,
Ober et al [24]. The finding is alarming since the American Heart
Association recommends that children with heart disease should
visit a dentist for the institution of preventive measures.
The lower frequency of dental visits in this study compared to
other studies in developed countries could be because of the reasons
that include the fact that; most of the caregivers are ignorant on the
importance of preventive dental care among the children with heart
disease. Most of the patients examined were of lower socioeconomic
status, therefore, could not afford the treatment. Also; the dental
facilities in Kenya are limited, inaccessible and most of them lack
skilled dental personnel who are well trained to offer treatment
to children with special needs. The use of other tooth cleaning
devices like the chewing stick was illustrated in this study. Majority
of the children who were using this device were mostly from rural
areas where other tooth cleaning aids may not be available. The
outstanding fact was that the children examined were from different
residential backgrounds. The patients who used the chewing stick
in this study had significantly lower dental caries experience than
those who used the toothbrush. The low caries experience in the
children who used the chewing stick may be because they could
not afford the snacks between meals. The low could probably be
explained by the fact most of the children who used the chewing
stick were from rural areas where the dental caries experience was
shown to be lower compared to urban centres possibly because of
the difference in the diet. Also, some studies have demonstrated the
cariostatic and bacteriostatic properties of some specific species of
trees, which are used as chewing sticks. It is also possible that a few
children who started to use the brush late in life after severe early
childhood caries had been established could have skewed the high
caries experience illustrated among the children who were using
the brush.
The caregivers’ aggregate oral healthcare practices did not
significantly influence the dental caries experience among the
children in the present study. The lack of differences in the gadgets
for cleaning the teeth may be due to the small sample size where there
was a loss of statistical power. Fifty-three (65; 4%) children whose
caregivers were classified as portraying “unfavorable practices”
had higher caries experience with mean dmft of 3.62±3.54 (n=53)
compared to 2.74±2.85 (n=8) among the children whose caregivers
reported “unfavorable practices” on oral care. The children who had
been to a dentist had a higher dmft than those children who had
never been to a dentist. This finding illustrates that children visit a
dentist when dental disease dental caries has already occurred and
that the majority of the treatment offered was curative to relieve
the symptoms, with little or no emphasis on preventive oral care.
The lack of focus on preventive oral care was further illustrated
by the high proportion of active, untreated caries component of
dmft compared to filled or extracted teeth. Despite the fact that
caregivers’ aggregate oral health care practices had no significant
relationship with the oral hygiene of the children as noted earlier,
thirteen children whose caregivers reported “favourable practices”
had lower plaque scores of 1.69 ±0.54. However, the plaque scores
of sixty-eight children whose caregiver’s had reported favourable
practices had a mean plaque score of 1.73±0.59 slightly higher.The
children who cleaned their teeth had significantly lower plaque
scores compared to those children who never cleaned teeth. The
children whose teeth were never cleaned were at high risk of
developing sub acute bacterial endocarditis when compared to
the children who cleaned teeth regularly. As during the tooth
brushing process, there is the mechanical removal plaque thus
reducing the possibility of increased bacterial colonization of the
plaque and reducing chances of bacteraemia during mastication.
It was noted the that toothbrushes were more effective in control
of plaque compared to the use of chewing sticks, though there
was no significant difference between the two groups. The results
of these study showed that children who had been to a dentist
displayed better oral hygiene than those children who had never
been to a dentist, though there was no statistical difference. The
difference perhaps indicates that the dentist visited previously
could have offered oral hygiene instructions on good tooth brushing
techniques. In addition to that, the caregivers’ aggregate oral
healthcare practices did not significantly influence dental caries
experience among the children. Those children whose caregivers
were classified as portraying “unfavorable practices “on oral care,
had higher caries experience with mean dmft of 3.62±3.54 (n=53)
compared to 2.74±2.85 (n=8).
The children who had been to a dentist had higher dmft than
those children who had never been to a dentist. The finding may be
rationalised that children who visited the dentist they did so when
dental caries had already occurred. The primary treatment offered
was curative to relieve the symptoms, with little or no emphasis
on preventive oral care. The situation was further illustrated by
the high proportion of active, untreated caries component of dmft
compared to filled or extracted teeth.
Conclusion
The utilization of oral health care and oral health practices of
the caregiver of the children was low, and only apparent used in
case of emergency mainly. The oral hygiene, gingival index and
dental caries experience in the study population was high.
Study limitations
The study was only for three months. Hence children who had
had appointments in the previous clinics were excluded. The small
sample size based in three cardiology clinics may have created a
bias. The clinic was limited to 3-23-year-olds excluding the older
children 13-17 this is the policy on how paediatric age cut off as
defined by the ministry of health.
Acknowledgment
We thank Professor Loice Gathece for contribution in the design
of the study. The Kenyatta National Hospital and the University
of Nairobi Ethics and Research Committee fors approval of the
proposal. Alice Lakati who helped in statistical work and Dr. E.
Kagereki and Dr. Kiprop for data entry. The Nurses and the staff at
the Paediatric Cardiac clinics at the KNH, Mater Hospital and the
Gertrudes’ Garden children Hospital for facilitating data collection
during the clinical examinations for the patients. We acknowledge
all the parents and children who participated in the study without
whom the study would not have been a success.
Read more Lupine Publishers Blogger Articles please click on: https://lupinepublishers.blogspot.com/
Read more Lupine Dentistry Journal Blogger Articles Please click on:
| https://lupine-dentistry-oral-health-care.blogspot.com/
Follow on Linkedin :
https://www.linkedin.com/company/lupinepublishers
|
Subscribe to:
Posts (Atom)
Lupine Publishers: Lupine Publishers | Post Endodontic Pain Reduction...
Lupine Publishers: Lupine Publishers | Post Endodontic Pain Reduction... : Lupine Publishers | Journal of Otolaryngology Research Impact Fac...